People select their career paths for myriad reasons. I began my career in medicine because I was curious about how human bodies work. What makes them sick, and how do we keep them fit and healthy in ways that maximize our individual life expectancies?
In truth, my motives were both altruistic and selfish. I absolutely wanted to be of service to others, but I also aspired to live a very long life of my own.
My point of view on that expanded, though, from a seemingly unrelated event: hiring a financial adviser. I had no money, just a pile of debt from medical school. Still, I thought it would be worthwhile to get expert advice on how to decrease my debt and develop wealth.
With great anticipation, I imagined the advice I would receive at my first meeting. What would I learn that would put me on the path toward financial independence? Imagine my surprise when my one action item at the end of the first meeting was to purchase supplemental disability insurance. What? No investment strategy? No debt payoff advice?
The simple fact shared with me that day was that you must first protect your most valuable asset: your ability to work. Without your health, everything is at risk—your livelihood, your future financial security, your sense of fulfillment, and your happiness. I started to see it.
That lesson stayed with me throughout my training in public health and in my everyday observations of the world, ranging from Apple founder Steve Jobs’s dying of pancreatic cancer to the establishment of the United Nations Sustainable Development Goals (SDGs) that all, in some way, aim to protect people’s health.
In the current coronavirus disease 2019 (COVID-19) pandemic, we hear about New York governor Andrew Cuomo debating a reporter about the importance of tackling the economic hardship caused by stay-at-home orders versus risking a potential rise in deaths due to increased COVID-19 infections. Compare that with a statement made by heart surgeon and television personality Dr. Oz about how reopening schools might result in a relatively low increase in the COVID-19 mortality rate but that it’s a trade-off some people might accept. How do we prioritize actions? Can we achieve some balance?
While I certainly do not have all the answers, we can explore those questions.
Let’s start with the notion of priorities. It’s not surprising that I will always prioritize health. I see it as essential to all other things in life. Even so, the concept of prioritizing health is complex and nuanced.
Health-care professionals, for example, prioritize differently than public health professionals do. In health care, the prime concern is always the individual who’s looking for help and advice. Doctors, nurses, and other allied health professionals are trained to be strong advocates for their patients, directing all necessary resources toward their optimal health care. But in public health, we think about protecting populations over individuals, ensuring that scarce resources are focused where they will do the most good for the community as a whole.
For example, if you had $10,000 to spend, and you could offer only one of two choices—either providing 10,000 vaccines to young children or helping an older man with chronic lung disease get better—which would you choose? Well, it depends on whether you are that man’s doctor or a public health professional.
This is precisely why we have both professions—health-care providers who focus on individuals, and public health professionals who focus on populations—each with its own bucket of funding. Separating these roles keeps priorities in balance.
With COVID-19, however, there is the unwelcome scenario (which has happened in some countries) in which a lack of balance between health care and public health priorities forces doctors to choose who gets ventilators if they are in short supply. Even thinking about having to make this decision highlights how location intelligence should be used to plan for resource allocation in anticipation of hospital surges.
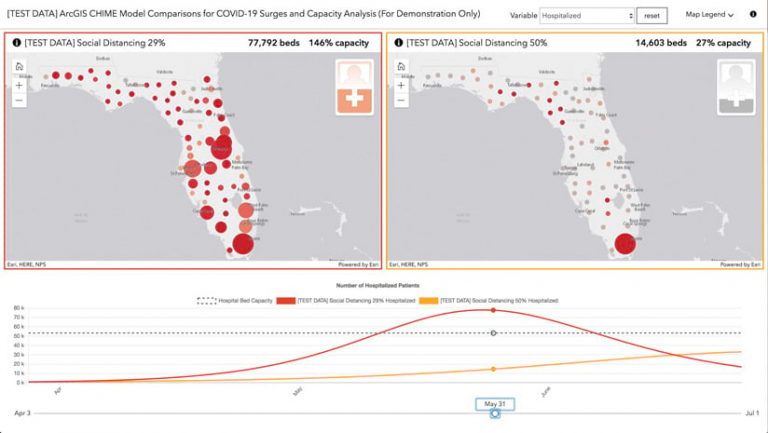
Spatial analysis and data visualization are enhancing surge capacity models that are meant to predict, over time, the number of people who will require hospital care, intensive care, and respiratory assistance with ventilators. Running those models to show various levels of adherence to social distancing policies and comparing the results with local health-care infrastructure capacity offer insight that can help plan for future needs. For example, if the current level of social distancing predicts a need for more hospital beds than a region has available, local leaders use GIS to site alternate treatment centers to augment capacity and better serve the community.
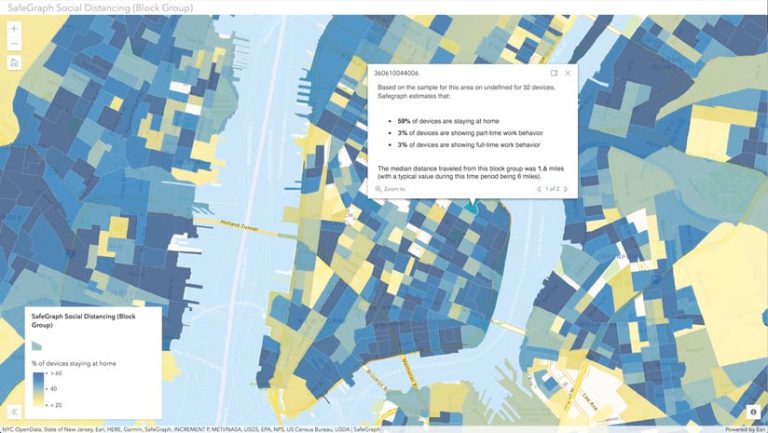
Public health priorities during this pandemic are foremost focused on prevention: how to decrease people’s exposure to the disease. The most common answer is social distancing.
In California, where I live, state-ordered social distancing began on March 19 and wasn’t given an end date. Some US states started reopening their economies at the end of April, while others sat tight. There is a tender balance between supporting people who face real economic hardship from not being able to work and addressing the need to protect ourselves, our families, and our communities from a rapidly spreading disease. I personally fear that I’ve seen that balance shift toward reopening too soon, despite continued growth in the US case count. It’s premature.
Still, I understand why this is happening. Public health organizations and health-care practitioners know that it is tough to sell prevention. Think about it. The health community gives out a lot of advice: eat healthy; exercise 20 minutes per day; and get your flu shots, colonoscopies, and annual checkups. Why? So you get nothing!
It can be a challenge to motivate people to work hard for an outcome that essentially adds up to nothing. The same applies to COVID-19, as people watch their businesses vanish, lose their jobs, or simply can’t survive on government stimulus checks. It’s tempting to throw caution to the wind and get back to work.
Is that okay, though? How do we balance severe financial hardship with every person’s responsibility to protect every other person from exposure to this disease? As Cuomo posited, “What is worse than death?”
The dilemma, in some ways, mimics the health-care-as-a-right versus health-care-as-a-privilege debate that’s gone on for years. When you look around the globe, people in many countries believe that their own health, wealth, and happiness are only as real as other people’s health, wealth, and happiness. Health care, in many of those places, is treated as a right. In other places, including the United States, people get the level of health care they can purchase. So health care is treated more like a privilege. These are longstanding philosophical and political belief systems that carry through to the policies we see today, culminating in the tug-of-war between protecting people’s health and reopening the economy.
These decisions vary significantly by geography. Policies for reopening should consider both rural and urban landscapes, since some level of social distancing is naturally achieved in rural settings. Is it safer to get back to work sooner in those communities?
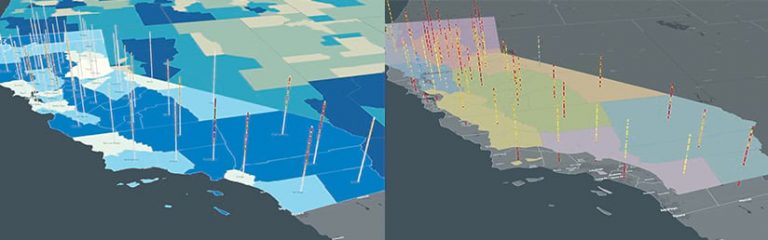
At the same time, doing an analysis of vulnerable populations could inform how urban areas open their economies. Can we develop a plan that protects older adults and people in nursing homes, assisted-living centers, and other kinds of communal habitations? How do we rationally consider racial inequity, economic vulnerability, and essential functions as well? Performing analyses that compare case data and social distancing data through space-time cubes across a landscape of vulnerability and regional boundaries can support better and safer decision-making.
There is no question that this pandemic qualifies as a disaster on all levels. As John D. Rockefeller once said, “I always tried to turn every disaster into an opportunity.” I suspect that the COVID-19 pandemic is one of those once-in-a-decade events that will change the world. The question is, how do we prioritize and balance those changes? Can we use lessons learned and federal funding to improve infrastructure, disease surveillance systems, data-sharing agreements, and the ability to respond with speed and precision? I think we can, and GIS should be part of that every step of the way.


