More than 300,000 babies are born each year with sickle cell disease (SCD), according to the World Health Organization. This inherited disorder causes red blood cells to become hard and sticky and distorts them into a crescent, or sickle, shape. This disrupts their flow through the body’s circulatory system. The cells also deteriorate quickly, causing a constant shortage of red blood cells, which carry oxygen from the lungs to the rest of the body.
St. Jude Children’s Research Hospital in Memphis, Tennessee, is a pediatric treatment and research facility that focuses on children’s catastrophic diseases. It is home to a regional pediatric SCD clinic that provides care for children with the disorder. Because St. Jude is a research institution, patients are involved in both therapeutic and nontherapeutic clinical trials. One of the nontherapeutic trials is the Sickle Cell Clinical Research and Intervention Program (SCCRIP), which follows participants with SCD throughout their lives to better understand clinical outcomes.
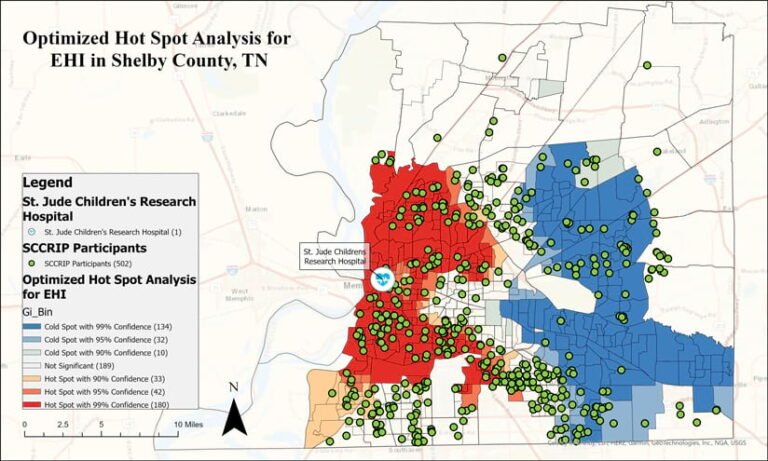
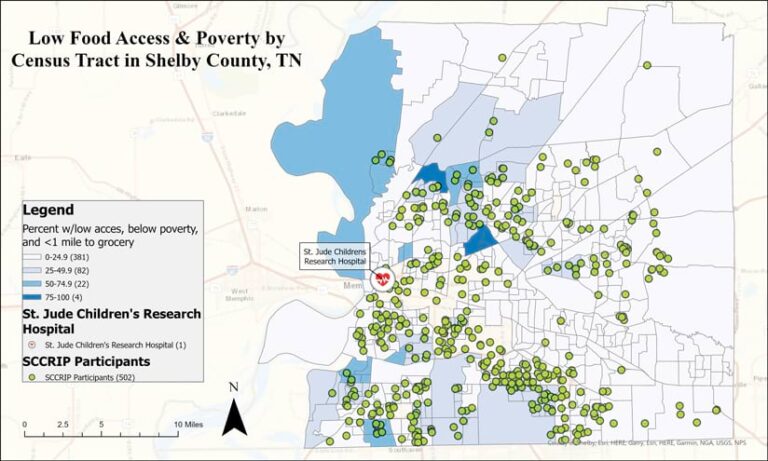
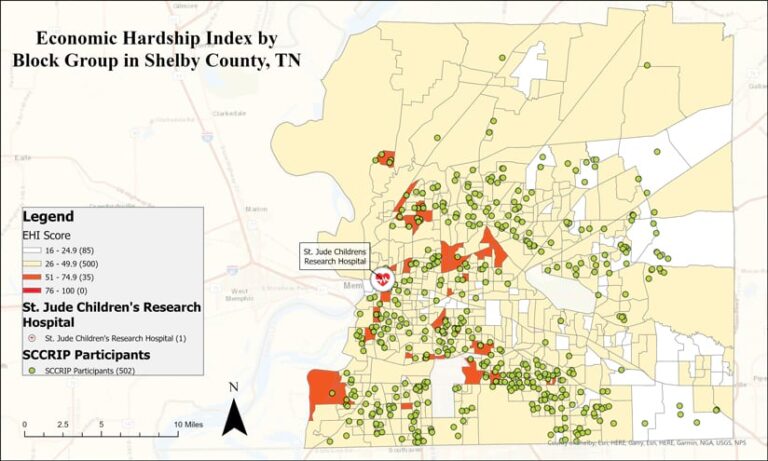
Recently, investigators at SCCRIP began to examine the social and environmental characteristics of the communities in which patients live. The analysis allows researchers to determine if there are factors, such as exposure to hazardous materials or the ability (and opportunity) to adhere to specified disease management programs, that may impact SCD treatment outcomes. ArcGIS Pro and several of its geoprocessing tools have been key to deriving location intelligence from the data and developing geospatial models to inform future treatment options.
Understanding Socioenvironmental Factors
Since SCCRIP began at St. Jude in 2014, several other prominent medical facilities have joined the program, expanding the number of patients participating in research initiatives. More than 1,300 participants, representing 92.3 percent of eligible patients, have enrolled in the SCCRIP protocol. The study group lives in the Southeast and Midwest regions of the United States.
“We are investigating the correlation between our SCD patients…and socioenvironmental factors in their respective communities that can affect treatment,” said Jason R. Hodges, director of clinical trials management in the Department of Hematology at St. Jude. “Through SCCRIP, we collect medical data in order to help us evaluate health outcomes in SCD patients, as well as identify their risk factors for adverse events. The overarching goal is to determine new ways to screen and treat patients with SCD, which will reduce the burden of their experience and increase their quality of life.”
Each year, SCCRIP institutes a data freeze, wherein its data team ceases new data collection and cleans and curates the data it already has. During this process, the team uses ArcGIS Pro to geocode participants’ addresses and obtain the census block groups in which they live.
“We then use indices, such as the Centers for Disease Control and Prevention’s Social Vulnerability Index and the Economic Hardship Index of those census block groups to understand what types of neighborhoods they live in,” Hodges explained. “This helps us determine the impact of the neighborhood environment on their SCD-related outcomes.”
In one project, researchers examined how access to food affects rates of acute health-care utilization among children living with SCD. The analysis found that individuals living in census block groups with limited access to better quality food had greater rates of emergency service visits and hospitalizations.
“ArcGIS was also used to analyze how living in a [census block group] with a higher level of economic hardship—including crowded housing, poverty, unemployment, low educational attainment, and alcohol or drug dependency—impacts adherence to SCD-related medication,” Hodges said. “Our analysis found that participants living in [census block groups] with greater hardship had evidence of lower medication adherence as assessed by certain lab biomarkers.”
Models Point Toward Tailoring Therapies
Fetal hemoglobin (HbF) is a type of hemoglobin that fetuses growing in the womb have in high levels but that declines when babies reach about six months of age. HbF red blood cells don’t form the sickle shape that causes them to get caught in and clog up the body’s circulatory system. Thus, SCD patients who have higher levels of HbF in their bodies have more rounded red blood cells in their circulatory systems and tend to experience fewer symptoms, which include severe body pain, leg ulcers, osteonecrosis (the destruction of bone tissue), and acute chest syndrome (a pneumonia-like illness that can be fatal). This is why many SCD patients take hydroxyurea medication. It increases their HbF levels and reduces the impact that sickled cells have on their bodies.
To better understand how patients’ social and physical environments affect the levels of HbF in their circulatory systems during hydroxyurea therapy, researchers at SCCRIP used ArcGIS Pro to develop a geospatial model.
“We hypothesized that patients living in neighborhoods reflecting a higher Economic Hardship Index [EHI] would have a lower HbF in comparison with those living in places with higher EHI scores,” said Hodges.
This would reflect hardships that make it difficult for patients to adhere to taking their hydroxyurea medication.
“The criteria included those with at least one higher-level HbF lab value collected [who] had received hydroxyurea treatment,” Hodges added.
The study group included SCD patients living in Shelby County, Tennessee, which represents roughly 85 percent of SCCRIPS clinical population. If the study produced interesting results, researchers would explore the hypothesis further.
Using ArcGIS Pro, researchers geocoded participant addresses and aggregated them by census block group. They then used the Cluster and Outlier Analysis, High/Low Clustering, and Hot Spot Analysis geoprocessing tools to identify clusters of patients who had high or low HbF values according to their lab work. Finally, researchers used the Geographically Weighted Regression tool to test explanatory variables for identified HbF clusters, such as patients’ ages, the duration of their hydroxyurea therapy, the EHI of their communities, and how far they live from a clinic. The researchers ended up confirming their hypothesis.
“Our findings point toward the importance of tailoring hydroxyurea therapy, including addressing potential barriers to hydroxyurea adherence that include contextual factors, such as the economic hardships observed in an individual’s neighborhood,” said Hodges.
Future Uses of GIS for SCD Research
As Hodges pointed out, thanks to SCCRIP’s participants and their families, investigators have been able to advance SCD research, expand care guidelines, and create better treatment options.
The team has high hopes for continuing to use GIS to analyze how SCD outcomes are affected by patients’ socioenvironmental factors. For example, SCCRIP collects location data related to the presence of asthma in its study areas, along with the number of hospitalizations SCD patients experience due to acute chest syndrome.
“I would like to examine how proximity to certain environmental hazards—heavily used roads, distribution centers, and superfund sites—impacts the health and treatment of our patients,” said Hodges.