I am putting my thoughts together on public health preparedness on the heels of all the remembrances from the events of September 11, 2001. I remember that day and the period just immediately following so vividly. Our lives changed dramatically: the way we traveled was altered, new departments were founded, and the way we evolved our response to a crisis changed from that day forward.
It is interesting how a jarring event is sometimes what is required to drive systemic change. We learned in the following days and months how much we did not know. We were forced to quickly learn what information was needed, how to bring back communications, how to mobilize teams, and what analysis would be needed to brief our cities and the entire nation. Most of the processes and information requirements that emerged had not been considered up to that point.
How 9/11 Changed our Response Efforts
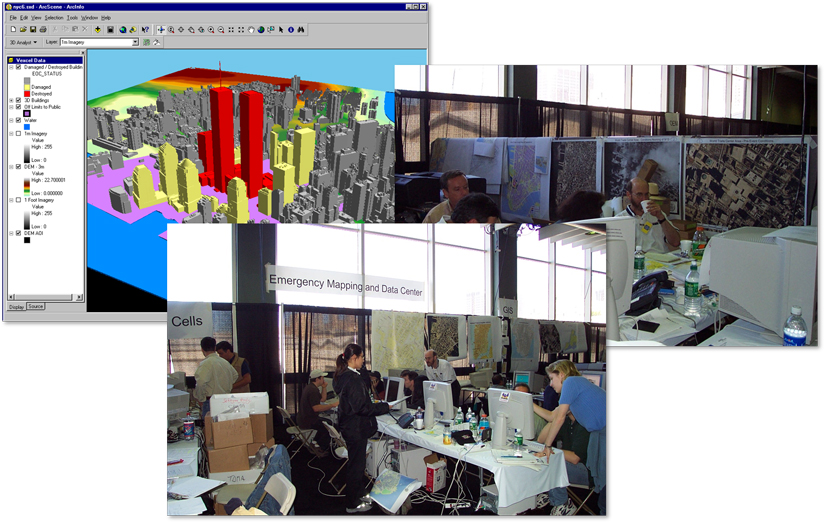
The events of that day forever changed the standard operating procedures for preparing for, responding to and recovering from a crisis. We consciously took the time to document the lessons we learned so we could share best practices with our peers. There was a significant new acknowledgement that responding to a crisis required the expertise from many disciplines, ranging from emergency management, law enforcement, public works, information systems, geographic information systems, and yes, public health.
Could This Lack of Preparation Been Avoided?
But one could debate that the public health elements did not experience the same level of focus and increase in resources, after 9/11, as their peers in other disciplines did. I actually wrote about this topic in April 2017 in a blog piece called Public Health Preparedness, Your Forgotten Partner. I suggested that public health professionals needed to be elevated as a partner in responding to crises. The argument I laid out revolved around how being prepared for a pandemic was as critical as being ready for a hurricane or fire.
I presented a call to give public health professionals a more prominent seat at the table of emergency operations centers. That was three years ago. Now here we are, facing a global health emergency. That same question can be asked again, do the health departments have a more prominent seat at the table?
Public Health Professionals Pioneer New Standards
Public health professionals have been thrust into the spotlight of the pandemic to offer leadership in the response and recovery efforts. The current status of a community’s health is the predominant indicator on situational awareness dashboards across the globe. Health departments have learned to be agile advocates for the public’s health. Data, information products, and new procedures like community contact tracing are being developed on the fly, and counties are leading the way. These efforts give way to pioneers in the field like Tri-County Health who serves Adams, Arapahoe, and Douglas counties in Colorado. Cobb County, Georgia demonstrated leadership with the establishment of one of the first COVID-19 resource hubs in the early days of the response. Their hub tackled everything from food assistance, to childcare for essential workers, to restoring the economy. The list of communities innovating and responding to this pandemic is impressive to say the least.
-
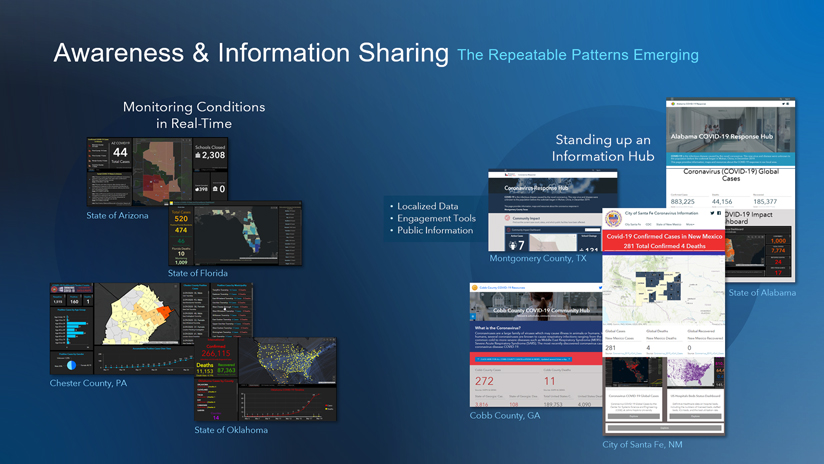
Organizations achieved awareness and sharing information by monitoring conditions in real-time and launching information hubs.
Three Things We’ve Learned to Date
Hopefully, one of the long-lasting impacts from the pandemic is the realization that health professionals need a more prominent seat at the table for emergency response. Another lesson I hope we take away is awareness of the must-have data, information products, and civic engagement tools that are needed in responding to health crises. Finally, that geographic information systems (GIS) has found renewed purpose in preparing for and responding to this pandemic. Much like it was touted after the response to the events of September 11.

A New Report Documents Best Practices
Unlike a response to a natural disaster, we are still learning as the COVID-19 pandemic continues. We are responding to an event that has a much longer response time, and with that comes new challenges we had not planned for. We are adapting as we develop definitions for ‘essential worker,’ aid economic stability, and work to protect voters on Election Day. We have an opportunity to stop and reflect on how far we’ve come. We can now look at and document activities that have become new standards in responding to the pandemic. My colleagues and I at Esri have documented the lessons learned to date in an industry perspective titled Strengthening Public Health with GIS. It shares common best practices and highlights the work that state and local governments have adopted. We hope you will find this industry perspective useful in strengthening your health-focused emergency response efforts.









