Note to readers: I’ve loaded this blog with several links to resources to help you dive deeper into the world of geospatial AI – so don’t forget to click on them!
Artificial intelligence is reshaping the entire health sector. From hospitals and health systems to public health departments, human services agencies, behavioral health programs, and emergency management, AI is accelerating how organizations understand communities, deliver services, and respond to emerging challenges.
Yet health is not just a matter of data—it’s a matter of place. Access to care varies by neighborhood. Environmental exposures and chronic disease clusters follow geographic patterns. Infrastructure, transportation, and social determinants shape who receives care and who is left behind.
Today, geospatial AI brings the full power of artificial intelligence into this geographic reality. It integrates machine learning, deep learning, computer vision, and natural language capabilities directly into ArcGIS—elevating both the science of spatial analysis and the experience of using GIS across the health landscape.
To understand this shift, it’s helpful to distinguish between two parts of the geospatial AI framework:
- GeoAI, which strengthens spatial analytics through machine learning—detecting patterns, forecasting risks, and extracting features from imagery.
- AI Assistants and AI Agents, which enhance the experience of GIS—helping users discover data, build maps, create surveys, and perform complex spatial tasks using natural language.

Together, these tools allow health organizations to see risk earlier, understand needs more clearly, and act more decisively. They also signal a profound shift in the future of GIS work itself.
Revealing Patterns That Matter for Health
GeoAI’s analytical capabilities help health organizations uncover patterns that traditional, non-spatial methods cannot. The foundation of spatial statistics rests on the idea that “near things are more related than distant things,” –a principle known as spatial autocorrelation. GeoAI amplifies this idea, using machine learning to detect statistically significant patterns in health data and understand why they occur.
Traditional statistics treat data points as independent, but spatial data rarely behave that way. GeoAI evaluates each location in the context of its neighbors, revealing patterns that matter for planning and intervention. Put simply:
Traditional statistics tell you if a relationship exists; spatial statistics can tell you where it matters and guide action.
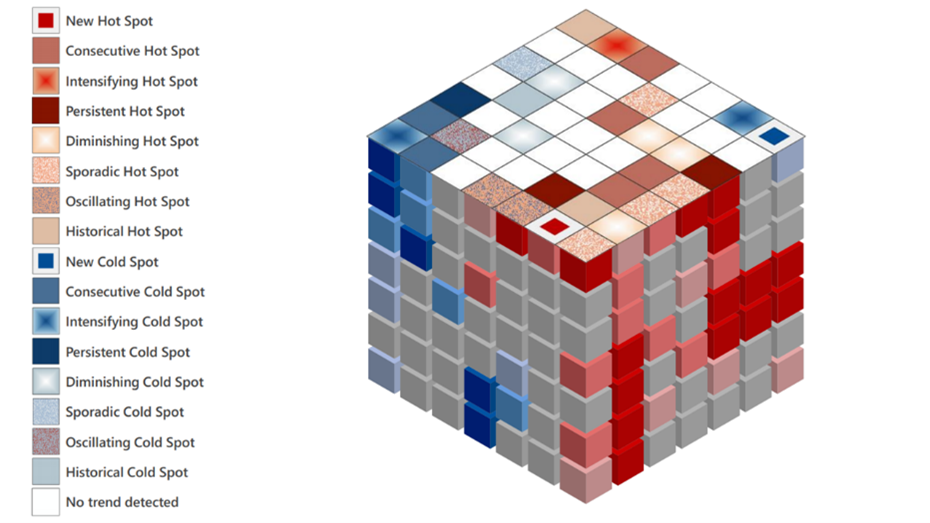
Hot spot analysis, for instance, identifies statistically significant concentrations of health events or conditions—such as chronic disease burden, ER use, behavioral health crises, medically underserved neighborhoods, environmental exposures, or service demand.
When time is added, these insights become even richer. The Space-Time Cube is a 3D data structure that enables organizations to understand how chronic disease trends evolve, where hospital admissions are intensifying, how homelessness patterns shift, or which communities experience persistent versus emerging environmental health risks. Change-point detection helps pinpoint when a trend shifts meaningfully—perhaps the beginning of flu season, the onset of rising overdose activity, or a sudden change in maternal health outcomes.
These capabilities support more timely and equitable decisions, whether in daily operations or long-term strategy. Leaders can move from reacting to crises to anticipating them.
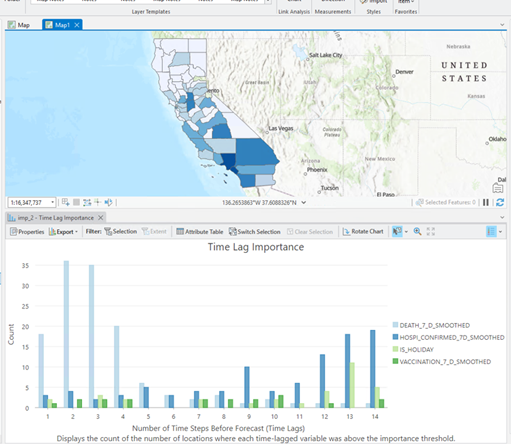
Predicting What’s Ahead
Regression models, such as geographically weighted regression (GWR), help organizations understand which factors matter where—clarifying local drivers of delayed care, poor outcomes, or gaps in access. Other GeoAI tools can fill in missing data, downscale coarse indicators, and generate neighborhood-specific forecasts that support targeted service delivery.
These approaches allow health systems, insurers, social services, and community-based organizations to tailor strategies to local conditions instead of relying on statewide or countywide averages.
Imagine forecasting ED surges, predicting where harmful algal blooms are likely to appear, or estimating likely death counts during a pandemic based on recent hospitalization data, mobility patterns, and even the presence of weekends or holidays.
Teaching Machines to ‘See’ Health Context
Computer vision–deep learning models trained to interpret images with human-level perception, is among the most rapidly evolving areas of GeoAI. It makes it possible to extract meaningful features from imagery at scale, which is particularly important in health, where the built environment, infrastructure, and environmental conditions shape health outcomes.
Tasks that once required weeks of manual review—such as tracing buildings in satellite imagery or assessing wildfire damage—can now be completed in minutes. More than 100 pretrained models available in ArcGIS can identify buildings, vehicles, road features, vegetation types, land cover changes, and more. Increasingly, these models support health-specific use cases.
This capability is particularly powerful across the health sector:
- Healthcare preparedness and facility management: Identifying vegetation near power lines, assessing roof damage, mapping facility footprints, or monitoring parking and traffic flow to improve wayfinding, safety, and operations.
- Environmental health: Detecting green pools where mosquitoes can breed, identifying septic systems or private wells needing inspection, monitoring hazardous dams, or spotting standing water after a storm.
- Behavioral and human services: Identifying heat signatures associated with homeless encampments for support during extreme weather, recognizing damage to homes after disasters, or tracking infrastructure that supports vulnerable populations such as blue-bay parking spaces or ADA curb ramps.
- Global health: Mapping informal settlements for vaccination campaigns, identifying roads and footpaths to estimate travel times to care, detecting thatched roofs or Attalea butyracea palms associated with vector exposure (key habitats for the triatomine bug Rhodnius pallescens, a Chagas disease vector), or identifying blue tarps signaling damaged homes after a hurricane.
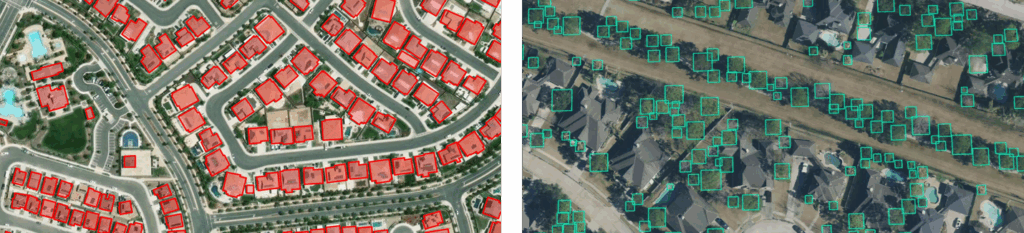
Some of these are happening today; others are emerging quickly as model-development workflows mature. Foundational models such as Segment Anything Models (SAM) along with next generation vision-language models further accelerate this work, making it easier to extract almost any feature from imagery.
Computer vision doesn’t just speed up workflows—it expands what health agencies can do.
Making GIS Accessible to Everyone in Health
Geospatial AI is not only advancing analytics—it is dramatically simplifying the experience of using GIS.
AI Assistants and AI Agents allow users to perform mapping and analysis tasks using natural language. A clinician, analyst, emergency planner, or program manager can simply describe what they want to see:
- “Map households within five miles of our clinic that lack a vehicle.”
- “Create a survey to assess community health needs.”
- “Show me where our behavioral health crisis calls increased this month.”
- “Find locations at high risk for floods in this municipality.”
Behind the scenes, the assistant identifies relevant data, configures parameters, and suggests next steps—always with human oversight.
These assistants and agents significantly lower barriers to entry, enabling more staff across an organization to engage with location intelligence. They are especially powerful for collaborative work across hospitals, clinics, emergency management, human services, and community partners who may not use GIS every day but need its insights.
How Geospatial AI Will Change Roles in Health
As AI becomes more integrated into GIS, the role of GIS professionals in the health sector will evolve—not diminish.
Routine map creation, survey building, and data discovery will increasingly be handled through AI-assisted workflows. That means GIS professionals can shift their focus to higher-value activities such as curating authoritative data, ensuring metadata quality, evaluating model performance and explainability, detecting and mitigating bias, developing governance frameworks, strengthening privacy and security, translating geospatial insights for clinical and operational audiences, and designing AI interfaces that help residents and partners ask and answer questions in natural language.
Geospatial AI democratizes access to spatial insight—but increases the need for human judgment, domain expertise, ethical review, and clear communication.
Rather than replacing GIS work, AI expands its reach and impact across the entire health ecosystem.
A Future of Connected, Insight-Driven Health Decisions
The promise of geospatial AI is not simply faster analytics or clever automation. It is the ability to see communities in context—geographically, environmentally, socially, and systemically.
With these tools, health organizations can understand the true reach of their services, providers can anticipate crises before they escalate, public health and human services agencies can better support populations, and organizations across the health continuum can prepare more effectively for emerging threats.
Geospatial AI helps answer the most essential questions:
- Where is need rising?
- Who is being missed?
- What risks can we predict and prevent?
- How can we allocate resources more equitably?
This is not science fiction—it is happening now, and the momentum is accelerating.
Responsible Use of AI
But innovation only becomes meaningful when paired with responsibility.
Transparency, explainability, bias assessment, privacy protections, and strong human oversight are essential if this technology is to strengthen public trust. With appropriate guardrails in place, the opportunity ahead is extraordinary.
Geospatial AI allows us to see patterns we could not previously see, anticipate risks before they emerge, and allocate resources with unprecedented precision. It helps ensure that interventions reach the right people at the right time, and that communities most affected by inequities are never left behind.
A Call to Action
The health sector stands at a pivotal moment. Geospatial AI is no longer optional—it is becoming foundational to delivering effective, equitable, and resilient care.
Now is the time for health leaders, analysts, GIS professionals, and community partners to:
- Build geospatial AI literacy within their organizations and across their teams
- Strengthen data governance, stewardship, and metadata practices
- Adopt transparent, ethical, and equitable design principles
- Explore practical applications of GeoAI and AI Assistants/Agents that support real-world health missions
- Invest in the workforce skills needed to guide, validate, and explain AI
- Collaborate across organizations to share successes, best practices, and lessons learned so the field can grow together
Health is shaped by place—but geospatial AI is reshaping how we understand that place and how we act within it.
The organizations that embrace this shift today will be the ones best positioned to improve outcomes, close gaps, and serve people and their communities with clarity, compassion, and precision.
If we can assist you on your geospatial AI journey to better health, contact us at healthinfo@esri.com.