I have called California’s Central Valley home for the last 27 years. The Central Valley is roughly 450 miles long and stretches from Sacramento in the North to Bakersfield in the South. It is known for its agriculture, oil production, and as a thoroughfare to travel between the Bay Area and Los Angeles. Geographically it is bordered by mountains east, west, and south, creating a bowl-like effect that produces some of the worst air quality in the nation. On most summer days you cannot see the mountains surrounding us.
In this environment, I developed asthma at a young age, making it extremely difficult to breathe normally. I had to learn about my body and its limits. I relied on medication to get through the day. Still, I did not let this chronic condition stop me from participating in sports or other activities. But like many, I have had some close calls and am constantly worrying about triggers like air quality, changes in temperature, and whether I’m laughing too much.
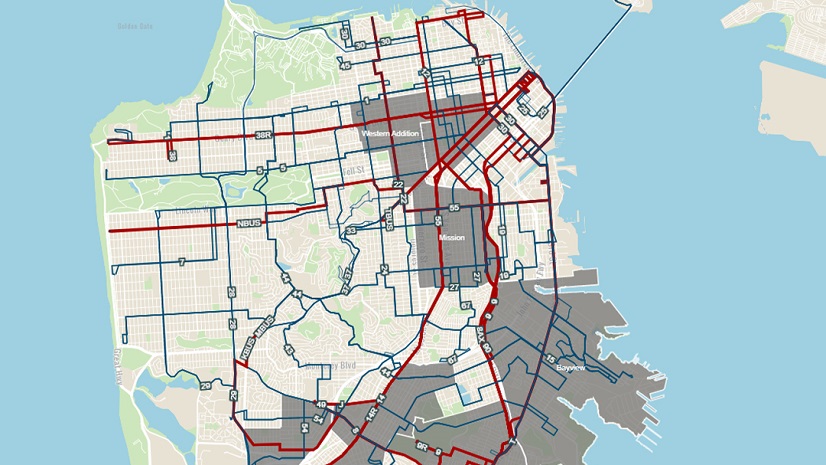
I’m not alone. California’s Central Valley has a comparatively higher prevalence of asthma than the rest of the state, making it a key area for assessment of inequities to adopt and implement solutions that enhance health equity then proactively. Geography plays an important role when it comes to air quality and health equity. With geographic information system (GIS) technology communities can pinpoint which areas are unjustly exposed, which are underserved, and where assistance should be prioritized.
If you have been following along with our Equity Across Industries blog series, you will find this piece inspiring as we learn how GIS technology continues to be at the forefront of health equity initiatives. I sat down with Esri’s Chief Medical Officer, Este Geraghty, to explore how health organizations are creating the world we want to see with GIS. Let’s dive in!
Sophia: How would you define equity within your industry?
Este: Well, Sophia, the CDC gives a succinct definition that resonates with me: “Health equity is when everyone has a fair and just chance to reach their best health.”
This concept, however, is a bit nuanced. What constitutes equity in one scenario may be very different from how we look at equity in another scenario. For instance, a clinical trial on ovarian cancer will have different clinical trial participants and equity considerations than one on prostate cancer. Similarly, interventions to enhance equitable resilience to extreme heat might focus on occupational status (outdoor workers) while pandemic preparedness planning may look at population risk and vulnerability according to home or vehicle ownership, financial means, race/ethnicity, and proximity to testing and vaccination resources.
Sophia: What organizations are successfully pioneering the equity effort in this area?
Este: Almost every health organization using GIS aims to enhance health equity. In our industry, some of the most common GIS workflows are to perform community health assessments and then map health outcomes to identify disparate and potentially inequitable patterns, perform analysis to discover root causes, and then apply interventions in a targeted and specific way.
That said, I do have some favorite examples. Milwaukee County, Wisconsin is a standout. They developed the EVE Model which evaluates vaccination rates against social vulnerability at neighborhood levels. They used this to prioritize vaccination messaging and resources in the places that had low vaccination rates and high vulnerability. They had such great success with improving vaccination rates that they applied the model to other issues. They’re currently using EVE to pit social vulnerability against opioid overdoses to determine the most equitable placement of harm reduction vending machines across their county.
Additionally, Health Plans such as the Inland Empire Health Plan uses GIS to ensure that their enrollees have proper healthcare access. Going a step further, they used this data to extend additional services to their members with the greatest needs.
Sophia: What data sets do health and human services professionals need to consider to enhance equity in this space?
Este: This is a great question because data is truly the foundation for any analysis focused on health equity. First and foremost, I think basic demographic data is essential: age, sex, race, ethnicity, education level, and income are all important. A key aspect of the data is that it needs to be disaggregated at a small enough geographic level to be able to unmask disparities that may exist. Too often, health organizations are getting their data at county or ZIP Code levels. What they really need are datasets available at a census tract or block group level to make progress.
In health, we use a framework for understanding the potential factors associated with poorer health outcomes called the Social Determinants of Health. This model suggests that we consider all the following categories as having an impact on health:
- Education access and quality
- Healthcare access and quality
- Neighborhood and built environment
- Social and community context
- Economic stability
So, I hope you get the idea that health is extremely cross-cutting – most aspects of our lives have some potential influence on our overall health and well-being for better and for worse. The Esri Living Atlas of the World is a treasure trove for collecting and using the data that’s needed to support health equity programs. Not only does it have a huge amount of demographic data at small geographies, but it also has various indices and indicators that can be used to support equitable decision-making, such as the CDC’s Social Vulnerability Index or the County Health Rankings from University of Wisconsin Population Health Institute and Robert Wood Johnson Foundation.
Let’s not forget that it’s vital to listen to affected communities. Decisions should not be about communities without the community’s input. Their lived experiences, captured as either quantitative or qualitative data, are invaluable for equitable decision-making.
Sophia: What federal requirements should be considered when addressing health equity?
Este: Actually, there are several federal requirements that support the advancement of health equity. I’ll name a few that particularly require a geographic approach:
First is the requirement for nonprofit hospitals to perform community health needs assessments. This came out of the Affordable Care Act in 2010. The requirement is implemented through the Internal Revenue Service and is meant to ensure that nonprofit hospitals use their tax savings to improve population health in the areas they serve. To do that, they must first assess community health needs and then create an implementation plan.
Second, I’ll note a more recent requirement that came from the White House in 2022 – the Justice 40 Initiative. This initiative is focused on environmental justice. The idea is that 40% of certain Federal investments must be applied toward disadvantaged communities that are overburdened by environmental impacts.
And the third federal requirement that I’ll mention is through the Centers for Medicare and Medicaid Services (CMS) and pertains to the concept of network adequacy. In this requirement, qualified health plans must ensure that their enrollees have adequate access (measured in both time and distance) to a primary care provider and multiple specialists. Incidentally, there are also network adequacy requirements from states that apply to a broader set of health plans across the country.
Most health organizations want to do the right thing when it comes to equity. Still, these regulations help align everyone’s efforts and set standards.
Sophia: Which GIS tools can organizations leverage to advance equity in this industry?
Este: I’d say, “all of them” with a wink! Obviously, I’m a firm believer in the notion that applied GIS is critical to solving health equity challenges. That said, there are some tools that shine in this endeavor.
ArcGIS Solutions: To make life easier for folks who need to accomplish routine workflows, Esri has connected several tools to create an easy-to-use end-to-end process. We call those “ArcGIS Solutions.” We have several that promote health equity workflows such as: Community Health Assessment Solution, Social Equity Analysis Solution, Immunization Outreach Solution, Warming and Cooling Center Solution, Homelessness Risk Reduction Solution and Opioid Epidemic Outreach Solution.
Esri apps: I mentioned before that it’s essential to engage communities in the discovery and decision-making process when it comes to health equity. Several GIS tools can support that engagement and the sharing of community voices like ArcGIS StoryMaps, Survey123, and ArcGIS Hub.
ArcGIS Analysis: Of course, using ArcGIS Online, ArcGIS Insights, or ArcGIS Pro will be foundational to any of the mapping, visualization and analysis work that needs to be done. Some analytic tools that I think are especially relevant to health equity include:
- Hot spot analysis – which looks for clusters that are significantly higher or lower than the mean value for an area. Say you want to look at something like teen pregnancies. You could use this tool to find out which neighborhoods in a city or county were experiencing higher than expected teen birth rates for that jurisdiction.
- Regression analysis – applying regression analysis geographically can help to differentiate which factors are important to creating observed inequities. That understanding helps ensure that the right resources go to the right places.
Creating Indices: We know that often health inequities arise from cumulative contextual burdens to individuals and communities. And so many health-focused organizations are creating composite indices to account for that. We have a great technical paper on best practices for creating these indices using ArcGIS. It’s a helpful resource to ensure that the consequences of every decision are carefully considered.
The last tool that I wanted to mention is an educational tool. There may be people out there that agree that tackling health inequities is a strongly geographic endeavor, but maybe they don’t have the GIS skills they need to accomplish some of this work. So, we’ve built a Health GIS Curriculum to help people learn the most common GIS tools in our industry. It’s all free AND it’s available in 7 languages, supporting inclusive learning as well.
Creating the World You Want to See
If organizations leveraged GIS technology to prioritize their work and create a more equitable environment, I may have avoided developing asthma all together. Communities such as the Central Valley are found everywhere, with geospatial analysis organizations can uncover these types of health disparities early on. The tools and resources covered in this blog provide you with the means to then operationalize your health equity initiatives and programs. We hope these examples empower you to adopt a location-based health equity plan.